The AIDS Foundation of Chicago and partners demand United Healthcare halt their practices and policies that discriminate against the LGBTQ community.
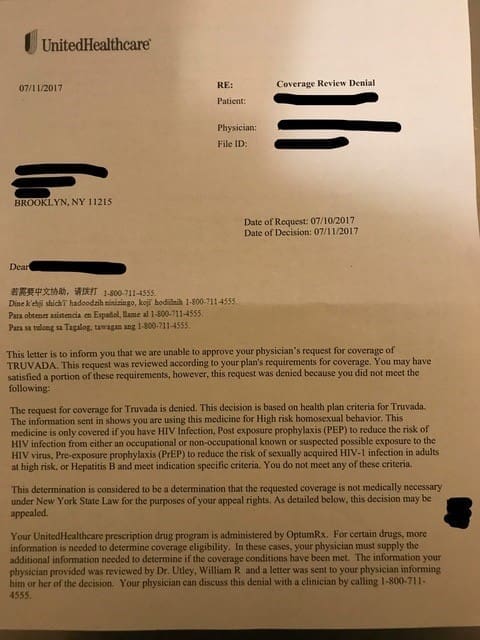
Earlier this year, United Health Care began to send members letters denying access to Truvada prescribed for Pre-Exposure Prophylaxis or PrEP. The reason for denial? According to the letter, shown in full below or click here to view, it was because the consumer was “taking this medication for High risk homosexual sexual behavior”. PrEP is a critical advancement in HIV prevention. UHC’s practices requiring members to receive PrEP through mail order pharmacies and denying PrEP without justification is not only discriminatory and dangerous – they are also illegal.
Read the full letter HIV advocates sent to UHC demanding they change their PrEP mandated prior approval process below.
Letter from United Healthcare Denying Access to PrEP
 |
 |
Letter from HIV Organizations to United Healthcare
August 4, 2017
Stephen J. Hemsley
Chief Executive Officer
David S. Wichmann
Office of the Chief Executive
President
UnitedHealth Group
P.O. Box 1459
Minneapolis, MN 55440-1459
Dear Mr. Hemsley and Mr. Wichmann:
We, the undersigned organizations, urge United Healthcare (UHC) to reverse the utilization management requirements that took effect July 1, 2017 for Truvada prescribed for Pre-Exposure Prophylaxis or PrEP.
Specifically, we believe requiring detailed documentation to request prior authorization every three months for Truvada prescribed for PrEP and requiring all members to use UHC’s mail-order pharmacy, BriovaRx, violates the Affordable Care Act (ACA)’s non-discrimination protections and federal and state laws barring mandatory mail order policies. We respectfully request a meeting to discuss the impact of these new policies on UHC customers.
PrEP is a critical advancement in HIV prevention that, when taken as prescribed, can provide nearly 100% protection from acquiring HIV infection. Stigma and discrimination are major barriers that have impeded uptake of this highly effective prevention intervention. In addition to violating multiple laws, the new policies have been implemented in such a way as to insult and disrespect UHC members. We have been shocked and appalled by the language in the coverage denial letters that are being sent to patients taking Truvada for PrEP and to patients living with HIV taking Truvada as part of a treatment regimen. The denials are contradictory and contain the type of inflammatory and judgmental language that contributes to the stigma that lesbian, gay, bisexual and transgender individuals and others face. In addition to written communications, UHC members have been subject to inappropriate and invasive questioning about their sexual orientation, HIV status and drug use by customer service representatives.
Excerpt from an OptumRx Denial letter:
“Your request for coverage for Truvada is denied. This decision is based on health plan criteria for Truvada. The information you sent in shows you are taking this medication for High risk homosexual sexual behavior. This medication is only covered if you have HIV Infection, Post exposure prophylaxis (PEP) to reduce the risk of acquisition from either an occupational or non-occupational known or suspected possible exposure to HIV, Pre-exposure prophylaxis (PrEP) to reduce the risk of sexually acquired HIV-1 infection in adults at high risk or Hepatitis B and meet indications specific criteria. You do not meet any of these criteria.”
We urge you to consider the points outlined below and immediately reverse the prior authorization restrictions implemented in July 2017.
UHC’s Policy Requiring Prior Authorization for PrEP Violates Non-discrimination Protections
The federal Medicaid Act and Section 1557 of the ACA prohibit discrimination on the basis of race, color, national origin, disability, age, and sex. Section §1557 prohibits insurance companies that participate in the state exchanges from discrimination based on these characteristics. The sex protections within the ACA have been interpreted to include gender identity, and sex stereotyping which many courts and federal agencies have implemented to also include sexual orientation. These protections extend to discriminatory drug benefit designs, including unjustified prior authorization processes. With specific regard to HIV medications, the court has ruled that placing arbitrary barriers on HIV medications constitutes discriminatory plan design. This applies to PrEP, which is primarily prescribed to gay, bisexual, or same-gender-loving men; black women; or transgender women.
UHC’s Prior Authorization Policy Is Restricting Access without Justification
We strongly object to the stringent and overly complex prior authorization documentation that is now required to request coverage of Truvada for PrEP. The medical providers prescribing PrEP are better positioned to determine the clinical appropriateness of PrEP for patients as evidenced by the communications that have occurred regarding this issue and the inappropriate denial letters UHC members have received. If prior authorization is maintained, we urge for the process to be significantly simplified and streamlined and for best practices to be followed. In particular, the approval period should be for 12 months, as is standard practice for medications that are prescribed for an extended period. The three-month cycle puts patients at risk of delays and medication interruptions and creates unnecessary burden to providers and anxiety for UHC members.
In order to protect against HIV acquisition, a patient must have consistent access to PrEP without interruption. Delays caused by UHC’s prior authorization approval put individuals at greater risk for acquiring HIV infection.
From a UHC Member:
“I have been on PrEP for three years and with UHC for the past year. I called in a refill of my Truvada to my local Walgreens on Saturday, July 1, with two pills left from my previous month’s prescription. I went to the Walgreens to pick up my prescription where I was told by the pharmacist that United Healthcare was requiring a prior authorization for my Truvada.
I called United Healthcare and they confirmed that a prior authorization was now required for Truvada and that a prior authorization request had already been sent to my doctor. I called the doctor’s office to find out if the prior authorization was approved. The office told me that the authorization was denied and I needed to call UHC to find out why. I then called UHC and asked if I could appeal the denial and I was told that I should call my doctor and have them call United Healthcare to start the appeal.
I called my doctor’s office and told them that I wanted to appeal the denial. The doctor’s office said that they need to ask me a few questions in order for the doctor to write a letter of appeal. I was asked how many men I have had sex with, was I a receptive anal sex partner, have a slept with HIV positive men, and if I had ever done crystal methamphetamine. I told the doctor’s office that I did not feel comfortable answering these questions.
I called United Healthcare and I asked to speak with a supervisor. The supervisor told me that it would take up to 15 days to do an appeal and five days to do a prior authorization once the HIV test was done. I told the supervisor that I was out of my Truvada prescription and I asked for them to cover a five day supply and they refused. I was also told that I would be required to fill my prescription through United Healthcare’s mail-order pharmacy.
This was an incredibly frustrating experience and I hope that United Healthcare addresses the barriers they created in having patients fill their Truvada prescriptions.”
UHC’s Mail Order Pharmacy Requirement Violates Existing Law
UHC is in violation of the ACA, 45 CFR § 156.122(e). The law requires any health plan required to offer Essential Health Benefits to allow enrollees to access prescription drug benefits at in-network retail pharmacies, unless there are specific safety or handling requirements that would preclude use of a retail pharmacy. Since July 1, UHC has repeatedly failed to provide an opt-out process for customers prescribed PrEP.
In addition to violating federal law, a number of states have statutes that bar mandatory usage of mail order. Georgia Code § 33-64-7-2, effective July 1, 2017, prohibits insurance companies that own pharmacy benefit managers from requiring their customers to use a mail order pharmacy. New York State’s Anti-Mandatory Mail Order Law similarly prohibits pharmacy benefit managers from requiring that patients purchase prescription drugs from a mail order pharmacy or pay an additional co-payment fee when such purchases are not made from a mail order pharmacy.
The mail order requirement is in violation of the 2014 Settlement Agreement arising from John Does I-V v. United Healthcare Insurance Company. The U.S. District Court of the Central District of California ordered United Healthcare to allow their customers taking HIV medications to opt-out of a mail order pharmacy requirement due to concerns about safety and privacy. The plaintiff class was concerned that their HIV status and sexual orientation would be inadvertently disclosed during delivery of their medications. UHC customers taking PrEP share those concerns.
Home delivery of medications to individuals in shared living situations or without secure mail receptacles puts UHC members living with stigmatized conditions or at risk for stigmatized conditions at unnecessary risk for stigma and discrimination. Truvada also is prescribed to treat HIV and discovery of the medication and other HIV medications threatens UHC members’ safety and privacy, potentially leaving them at risk for violence and discrimination.
From a UHC member:
“Since December 2015 I have picked up Truvada at a local retail pharmacy by opting-out of the mail-order requirement and having UHC grant an exception to deliver my meds to this specific pharmacy. Now due to the changes that went into effect 1 July 2017 (which I am still unsure what those changes are), the customer service representatives at UHC tell me that I can no longer opt-out. I repeatedly told them that I have major privacy and security concerns over receiving my PrEP through the mail, and they just now seem to be interested in looking to grant me another exception. I am out of PrEP as of tomorrow, and UHC will be responsible for this outrageous and unacceptable lapse in coverage. I am in school to become a physician and this process is mind-bendingly confusing even for me – I cannot fathom how someone without my level of health literacy could navigate these added barriers. This is an attempt to confuse and intimidate a vulnerable population into forgoing the lifesaving preventive services we deserve.”
Conclusion
In response to these concerns, we urge UHC to:
1. Remove the prior authorization requirement for Truvada for PrEP. If a prior authorization process is maintained, it should be significantly streamlined, invasive personal information should be removed, and be approved for a 12-month period.
2. Remove the mail-order pharmacy requirement and allow customers to opt-out.
PrEP is an effective prevention intervention that can help to stop HIV in its tracks. UHC members should not be denied access to this highly effective HIV prevention tool.
UHC’s prior authorization process is discriminatory and unnecessarily complicated, and the mail order requirement is illegal. For the reasons stated above we believe these actions are discriminatory in nature and reserve the right to pursue this matter further by filing a complaint with the U.S. Department of Health and Human Services Office for Civil Rights, charging unlawful discrimination under the Affordable Care Act’s non-discrimination protections.
We reiterate our request to meet with you immediately to discuss the UHC prior authorization policy for PrEP. We look forward to your response within 10 business days.
To schedule a meeting or to resolve questions regarding this letter, please contact:
Ramon Gardenhire, AIDS Foundation of Chicago, (312) 334-0928 or [email protected]
Benjamin Brooks, Health HIV, (202) 507-4737 or [email protected]
Respectfully,
AIDS Foundation of Chicago
AIDS United
APLA Health
Association of Nurses in AIDS Care
Health HIV
Human Rights Campaign
HIV Medicine Association
National Coalition for LGBT Health
National Alliance of State and Territorial AIDS Directors
New York City’s Lesbian, Gay, Bisexual & Transgender Community Center
Project Inform
The AIDS Institute
San Francisco AIDS Foundation
Treatment Action Group

